Lessons Learned at the Interface of Medicine and Psychiatry
The Psychiatric Consultation Service at Massachusetts General Hospital sees medical and surgical inpatients with comorbid psychiatric symptoms and conditions. During their twice-weekly rounds, Dr Stern and other members of the Consultation Service discuss diagnosis and management of hospitalized patients with complex medical or surgical problems who also demonstrate psychiatric symptoms or conditions. These discussions have given rise to rounds reports that will prove useful for clinicians practicing at the interface of medicine and psychiatry.
Prim Care Companion CNS Disord 2025;27(1):24f03823
Author affiliations are listed at the end of this article.
Have you ever had a patient suffer so much that you wanted them to die? Have you wondered whether such thoughts and feelings are acceptable? Have you been uncertain about how you could manage your guilt over such thoughts? Have you been unsure about how to best advocate for a patient whose medical care is futile? If you have, the following case vignette and discussion should prove useful.
CASE VIGNETTE
Ms A, a 62-year-old woman with idiopathic pulmonary fibrosis, underwent bilateral lung transplantation. Although she had been an excellent candidate for transplantation, her course was complicated by initial primary graft dysfunction (that required ventilatory support and extracorporeal membrane oxygenation [ECMO]), multiple bouts of infection (including fungal pneumonia), renal failure (that required dialysis), mesenteric ischemia (that led to an ostomy), severe deconditioning, and ongoing use of pressors to support her blood pressure. Nine months after her transplant, she remained in the intensive care unit (ICU) and still required ventilatory support and dialysis. For the last 2 months, she had struggled with delirium due to multiple medical conditions. Her family (a husband, 2 sons, and grandchildren) stayed by her bedside and hoped for her full recovery.
Throughout her ICU stay, her ICU and transplant teams as well as multiple consultants from other disciplines (eg, nephrology, infectious diseases, neurocritical care, psychiatry, and occupational and physical therapies) experienced myriad emotions (eg, anger, irritability, and guilt) in response to prolonging what seemed inevitable, seemingly without consideration for what Ms A had wanted or would want, and confident that she would not survive her hospital stay. However, some members of her ICU and transplant teams continued to express hope for her recovery. Others thought that a 1-year survival for transplant recipients was an important contributor in the primary teams’ decision-making. Several of her health care providers tried to avoid caring for her, feeling that their actions were futile and contributed to her suffering.
DISCUSSION
What Is Meant by Medical Futility?
“Medical futility” is not esoteric bioethical jargon. Its widely cited definition is “A medical act is futile if (based on empirical data) the desired outcome, although possible, is overwhelmingly improbable.”1(p199) When determining whether an action is futile, it is important to consider whether the intended outcome is desirable. Ethicists refer to such reasoning as the qualitative aspect of futility, wherein an intervention’s burdens outweigh its benefits or will fail to provide the patient with a quality of life worth prolonging.2 Nevertheless, medical care that does not offer any meaningful hope of recovery is now widely understood to be futile, and this notion has been critical to the growth of hospice services.3
Clinicians must also assess the probability that an action will achieve the desired goals. Recent literature refers to these probabilistic considerations as the quantitative aspects of futility.2 However, medicine rarely deals with certainties, and quantitative futility does not demand that the desired outcome be impossible, only highly improbable,4 and no professional organizations have proposed a statistical threshold for determining futility. Even the most evidence-based providers integrate mechanistic reasoning and empirical data. Thus, the quantitative definition of futility does not refer to objective statistics but to the subjective prognostication of a reasonable and well-informed clinician.
Thoughtful appreciation of the qualitative and quantitative aspects of medical futility informs sound decision-making. The field of neuro-prognostication offers an illustration. Brain death, a concept formalized by Beecher,5 described a state in which both types of futility are maximized, wherein the odds that treatment could result in any patient experience whatsoever are so low that no treatment is warranted and harvesting of organs becomes ethical. However, more complicated reasoning must be applied to patients in a vegetative or a minimally conscious state.6 Early in the course, critical care services have a high likelihood of preserving life, but there is a high degree of uncertainty regarding the eventual quality of life. As time passes, certainty about the level of recovery increases, but medical complexity often also increases, creating more quantitative uncertainty.7 As such, in the weeks shortly after a neurologic injury, care is often withdrawn due to concerns about qualitative futility (low likelihood of obtaining a desirable outcome), but years into the course, care is typically withdrawn due to quantitative futility (the low likelihood that any intervention will correct the accumulating medical complications). Conflict arises when the language used becomes imprecise, such as when providers argue that the resuscitation of a neurologically injured patient would be futile, implying that it would be ineffective (quantitative futility) when the underlying reasoning is that the patient’s quality of life would be too poor to justify intervention (qualitative futility).8
Who Decides That Medical Care Is Futile?
Prior to the 1970s, when medical futility was not even considered, medical paternalism dictated that physicians should determine the nature and extent of care provided. Over the following decades, the medical system slowly transitioned to a model that involved more patient autonomy, which called into question who should determine when a patient is at the end of their life. However, providers may disagree with one another. As patient autonomy grew, physicians transitioned from their role as sole decision-makers to shared decision makers.9 Advance care directives and health care surrogates have facilitated this conversation even when the patient was unable to participate. Moreover, physicians should not assume that all patients are incapacitated or unable to participate in end-of-life discussions merely because they are in the ICU or ventilated.10 These decisions often depend on the input of family members who are acting as surrogates to convey the patients’ wishes.11
Although these conversations often provoke anxiety among physicians, defaulting to a formulaic script or eschewing a shared decision model should be avoided. Recommendations published by the Ethics Committees of the American College of Critical Care Medicine and American Thoracic Society recommend that “Clinicians should engage in a shared decision-making process to define overall goals of care (including decisions regarding limiting or withdrawing life-prolonging interventions).”12(p5) Nevertheless, surveys of ICU physicians and family members of ICU patients found that a physician-driven approach was more common than true shared decision-making.11
When patients or their family members dispute the determination of medical futility and are opposed to withdrawal of care, patient advocates and/or an ethics committee should become involved. Further exploration of patients’ values and life stories may resolve these differences of opinion.
How Can a Ventilated or Delirious Patient Be Assessed for Capacity to Make Medical Decisions?
Assessment of capacity to make medical decisions in ventilated or delirious patients requires a thoughtful approach due to the unique challenges that these conditions present. Capacity refers to the patient’s ability to understand the relevant information about their medical condition, the proposed treatment options, and the consequences of accepting or refusing those options. It also involves the ability to communicate a choice based on rational reasoning. Assessment of capacity requires a multifaceted approach that balances clinical assessment, communication strategies, ethical considerations, and legal frameworks. The assessment should be tailored to the patient’s condition to ensure that decisions are made in the patient’s best interest when the patient is unable to make their own decision.
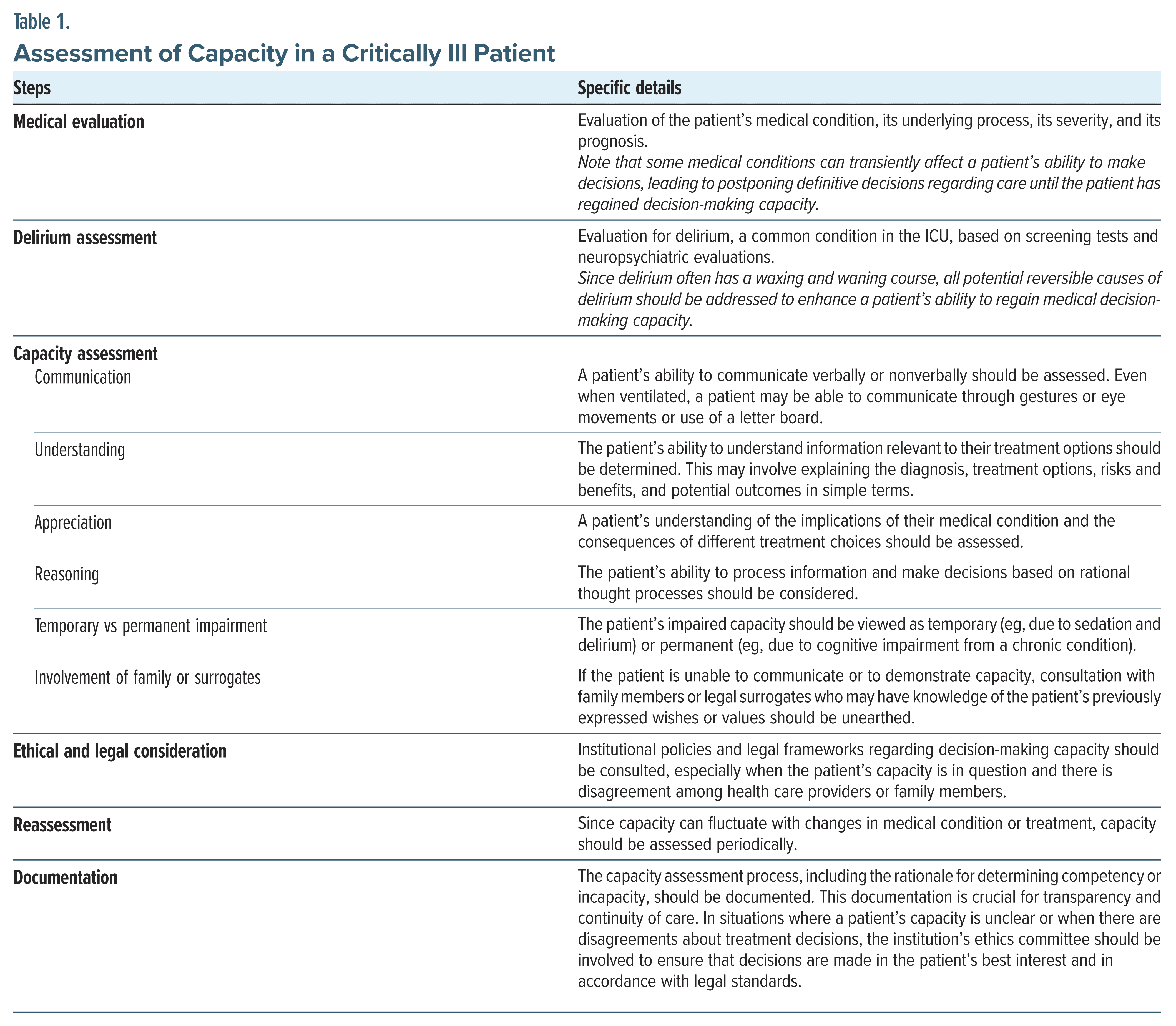
The capacity assessment involves evaluating whether the patient can understand the relevant information, appreciate the medical situation and its consequences, reason about treatment options, and communicate their choice coherently. Mental status and thus capacity to participate in the medical decision-making process among critically ill patients may be influenced by a variety of factors, chief among which are the underlying medical processes (eg, renal failure that might cause encephalopathy affecting the patient’s ability to think rationally), the nature of the medical treatment (eg, the use of steroids, opioids, and sedatives that might impair a patient’s decisional capacity), the patient’s lifetime experiences (eg, a patient’s experience with the illness or death of their parents that might color their willingness to undergo a similar process), and, finally, the experience of delirium. Delirium is common among critically ill and ventilated patients. Its development is likely to alter or impair a patient’s ability to think clearly or to apply adequate reasoning. Assessment of a critically ill individual should include several elements (Table 1).13–15
What Happens When Clinical Decisions Are Influenced by the Needs of the Transplant Program?
The development of transplant programs serves the needs of the community by providing life-prolonging and life-saving treatments to patients with end-organ damage. These programs are regulated by bodies that ensure fairness, equity, and ethical practices that are set through quality metrics.16 However, the need to excel at these metrics, particularly graft and patient survival at 1 year, can conflict with individual clinical decisions.
Transplant physicians often face a dilemma between their ethical duty to do no harm and the pressure to meet strict regulatory metrics. Both the United Network for Organ Sharing and the Centers for Medicare and Medicaid Services track 1-year adjusted mortality rates.16,17 Programs that do not meet specific benchmarks face the risk of audits, probation, loss of contracts with private insurers, or even being barred from performing transplants.18 High-profile cases in the media have highlighted how some transplant centers prioritize these metrics over patient well-being, striving to meet the 1- year survival mark. This creates ethical tension, as the primary goal should be patient-centered care, rather than achieving statistical targets.
Transplantation is an expensive intervention; according to the Milliman research report in 2020, the average costs for a kidney transplant, liver transplant, and heart transplant were $442,500, $878,400, and $1.66 million, respectively, in the United States.19 Quality metrics, such as graft and patient survival rates, are essential for maintaining funding and support for transplant programs. The high cost of transplants makes it crucial for programs to show successful outcomes to secure insurance reimbursements and hospital backing. Failure to meet these metrics can jeopardize the program’s existence, thus affecting future patients who might benefit from these services.
In cases of posttransplant complications leading to additional organ damage or prolonged ICU stays, a patient’s quality of life may be severely compromised. Transplant recipients can become chronically critically ill,20 which presents complex ethical challenges. Teams and family members alike wonder if invasive treatments without clinical improvements convey more discomfort and suffering.18 This situation often results in moral distress among medical teams, who must balance the principles of beneficence and nonmaleficence with the practical need to preserve the transplant program’s reputation.
Balancing individual outcomes and care with the need to preserve transplant programs for the greater good can be challenging. It is not uncommon for teams to be divided, with some advocating for relief of a patient’s discomfort and distress, even if that leads to a palliative approach. Others may remain optimistic about the success of their interventions and endeavor to further prolong the individual’s life. Teams that have experience in dealing with these situations tend to provide support and structure, fostering an environment where difficult cases can be discussed, emotions aired, and ideas brainstormed to narrow the gap between patient interests and the needs of the transplant program.
In dysfunctional groups that fail to provide space for discourse and instead employ an autocratic leadership that dissuades discussion, moral distress can be exacerbated. Some teams consider palliative care a “bad word,” that is often whispered in hallways, equating it with hospice care and hence an antithesis to the life prolonging transplant. In such circumstances, bioethical services can be consulted to ensure that practice is ethical. Developing support structures, such as bioethical consultations and open team discussions, can help narrow the gap between patient interests and program needs, ensuring that ethical practices remain at the forefront of clinical decision-making.
Is It Acceptable for Clinicians to Wish for Their Patients to Die?
Clinicians are humans with complicated thoughts and feelings that arise when caring for patients, especially those who are critically ill. Instead of judging one’s feelings or thoughts as “good” or “bad” or “acceptable” or “unacceptable,” clinicians might be better served by noticing and naming their feelings and understanding what they signify. Acknowledgment of these feelings, even the most uncomfortable ones, can help guide actions instead of blindly reacting to them.
Noticing that a clinician is deeply distressed by interactions with a patient or their family and wishing that a patient would die can be an expression of empathy while watching a patient and their family suffer when medical care is futile. Wanting a patient to die might reflect one’s guilt in prolonging a patient’s care and suffering or indicate one’s helplessness and hopelessness about the patient’s situation, or a clinician’s own wishes and ideas about their own quality of life, thus displacing their own wishes and values on to their patients.
The best approach to such thoughts and feelings is to notice, name, and attempt to understand their origin and meaning. When clinicians fail to pay attention to their feelings, they risk acting upon them unconsciously. Importantly, not all complex feelings should be shared with the patient or their families, as such communications can be misinterpreted in real time or in hindsight. Moreover, when clinicians identify, acknowledge, and reflect upon their feelings and when they discuss these reactions with colleagues, their interactions with complex patients and their families can become more intentional and nuanced.
How Can Clinicians Learn to Approach End-of-Life Discussions and Decisions in the Setting of Conflicting Staff Views?
The conflicting views regarding patient care have often been described in the literature on interpersonal conflict within health care, particularly within the ICU setting. Studies on ICU conflict have found that common sources of conflict center on poor communication, goals of treatment, and end-of-life decision-making.21–24 These conflicts contribute to clinician burnout, increase the risk of medical errors, and decrease patient and family satisfaction with care.22,23 Various approaches to mitigating conflict include self-reflection (eg, “Which of my biases am I bringing to these discussions?” “What are my knowledge deficits, skill limitations, and beliefs regarding death and dying?”).21
To combat disagreement, open communication among staff is encouraged, although difficult.23,24 Communication can be enhanced by having in-person conversations, scheduling proactive and regular case conferences that involve representatives from all disciplines, and creating educational opportunities driven by multidisciplinary staff.23,24 Optimizing communication improves success for other conflict resolution approaches, as well as acknowledging and discussing prognostic uncertainty.18,21,25 Open dialogue around differing opinions and data on prognosis allows for interdisciplinary team members and family members to understand divergent viewpoints and informed decision-making.18,25
It is often helpful to highlight ethical principles of beneficence and nonmaleficence during end-of-life discussions and to ensure that these principles are considered.18,25 Is the patient’s autonomy being considered and respected as part of the shared medical decision-making process? Are any advance directives being respected? In the case of lung transplant and nontransplant providers, are teams examining all systemic pressures that are influencing their decision making, such as program metrics?18 Lastly, the proactive engagement of an impartial third party, such as an ethics consultation, can help establish a forum to facilitate discussion.18,25
How Often Do Complex Cases Result in Disturbing Discussions?
Since everyone dies, all patients eventually face a point at which further medical care is futile. When futility is appropriately identified, the patient, family, and clinical team usually collaborate to adjust goals without experiencing disturbing conflicts. Although conflicts can arise in any setting, they tend to occur more frequently in ICUs when patients experience protracted critical illness.
Review of lung transplantation data offers a helpful perspective, given its association with complex and prolonged hospitalizations, with extended periods of ECMO, intubation, tracheostomy, and tube feedings. While transplant evaluation research accounts for the likelihood of 1-year survival, a measure of quantitative futility, qualitative aspects (such as posttransplant quality of life or even the likelihood of eventual discharge to home) have not been systematically studied.
Further, while a variety of factors (including dialysis dependence and stroke) predict death before discharge, mortality remains less than 50% even in these populations.18 Given this context in which quantitative futility rarely occurs, and qualitative futility appears common but has not been the subject of rigorous research, tension can develop between quantitative and qualitative notions and be disturbing for patients, families, and providers.
Who Can You Turn to When Uncertain About What Path to Take?
Whether one is acting as the primary care provider or consultant, caring for a critically ill individual can be stressful and isolating. Physicians frequently question whether care is medically futile, ie, treatment has not led to meaningful improvement in the patient’s condition and the patient is likely to die. This can lead to a sense of dread when broaching goals of care discussions or even doubt about next steps in care. Worse yet is when there is disagreement about the patient’s treatment plan.Fortunately, there are multiple options for seeking consultation.
Although ethics and palliative care teams frequently consult in critical care settings, this was not always the case. It was only 50 years ago when the controversial case of Karen Ann Quinlan (a woman in a persistent vegetative state whose family and the hospital disagreed about discontinuing her care) stimulated the concept of an “ethics committee” in hospitals.26 Later in the 1990s, palliative care similarly rose to the forefront.26 When a physician is uncertain about the next steps in a patient’s care, it is appropriate to engage both palliative care and ethics consultations.26,27 Each service can broach the goals of care discussions with patients, families, and providers. Palliative teams may serve a role as an “insider,” acting as a consultant on a case with the potential to offer more than goals of care and strategies for relief of distress.26,28 Palliative care teams also include hospice services. Both palliative care and hospice care share the goals of reducing stress and providing symptomatic relief, while they differ in that hospice care is delivered when further curative options are no longer available and global palliative care can be combined with treatment. Ethics committees, on the other hand, may not include medical personnel and may have a more circumscribed role, acting as an “outsider” without having to deliver patient care.26 Which service is consulted often depends on institutional policies and traditions as well as team dynamics, with universal support of early family meetings and goals-of-care discussions.
If a patient or family continues to insist on additional medical interventions despite their futility and the involvement of ethics and/or palliative care, physicians are not obligated to provide treatment.29,30 This practice is supported by numerous professional organizations, including the American Medical Association, as well as by legal statutes.29–31 Hospital administrations often have policies surrounding the provision of medically futile care, including processes for navigating discussions with patients and families.31 Physicians should consult with the hospital’s risk management team or legal office if such situations arise and document the rationale for decision making and obtaining additional consultations.
Are End-of-Life Discussions Held Only in ICUs?
End-of-life conversations are part of a fluid and mutable process that may begin years before critical illness strikes, even when a patient is discussing their wishes with family members, or when completing an advance health care directive. Such conversations are increasingly common between patients and their providers. Among Medicare decedents in 2015 compared to 2000, despite ICU utilization in the final month of life increasing and then plateauing at 29%, the proportion of deaths that occurred in acute care hospitals decreased from 32.6% to 19.8%, respectively. Moreover, a higher percentage of patients are dying outside of hospitals. This pattern matched a corresponding rise of decedents passing away while receiving hospice services, dramatically increasing from 21.6% to 50.4%. Of those who entered hospice at the end of life, only 40% made the decision following an ICU stay.32 These shifting demographics suggest that for most patients, the conversations to withhold or withdraw aspects of treatment are happening outside of ICUs.
As hospice care prioritizes comfort care over curative treatment, conversations to enter hospice can be used as a proxy for conversations regarding withdrawal of or withholding care. While roughly half of hospice referrals are from acute care hospitals, over one-fourth come from nursing homes or assisted living facilities, with the remainder being referrals from the community.33,34 Hospice referrals from the community had a higher prevalence of cancer diagnoses than those referred from the hospital, suggesting that patients with cancer are more frequently having end-of-life care plans independent of the acute care setting.33 However, even in cases of chronic and incurable stage IV cancer, the impetus for these conversations is usually an acute decompensation rather than the prognosis or the diagnosis itself.34
When Should a Patient First Assign Their Health Care Proxy and Create a Living Will?
A health care proxy and a living will serve as advance directives that guide decision-making surrounding medical interventions.35 When an individual is unable to communicate their preferences due to illness/injury, a designated health care proxy can make medical decisions on the person’s behalf, while living wills are written, legal documents that elucidate the individual’s preferences regarding medical treatment.35 Advance directives should be completed before an individual loses decision-making capacity due to illness or injury. An international consensus paper recommended that individuals can engage in advance care planning (at any life stage), but that its content should be more targeted as an individual’s health worsens or as they age.36
Data are mixed on whether advance directives and more broadly advanced care planning, improve patients’ quality of life or goal-concordant, end-of-life care. Factors related to advance care implementation include a lack of appropriate legislative frameworks, insufficient and varied physician and other provider training, inadequate accessibility of advance directives in medical records, multifactorial stressors that impact surrogate decision-makers, and dynamic changes in patient preferences that are based on multiple health determinants (eg, age, physical function, and social economic stressors).37–39 However, varied advance care interventions, including iterative, facilitated discussions and clear written directives, are associated with positive outcomes in patient/surrogate satisfaction with communication and care, as well as decreased surrogate and clinician distress.37 Thus, clear advance directives and repeated advance care discussions may help to decrease clinician burnout and provide surrogate support for patient care.
Primary care clinicians are well positioned, given their relationship with patients and their families, to obtain advance directives and to document discussions about patient preferences and the rationale for their decisions. This process helps the teams that care for these patients in critical care environments to provide care that is consistent with the patient’s values and goals.
Does Conducting End-of-Life Decisions Contribute to Burnout?
Burnout is a widespread occupational syndrome that affects health care workers; it leads to emotional exhaustion, detachment from work, and compassion fatigue.40 High stress environments such as ICUs are a breeding ground for distress, with up to 50% of ICU health care staff afflicted.41 ICUs and transplant units are filled with patients who have a high mortality rate and staff who work long hours providing intense patient care, making critical decisions, and monitoring patients closely to ensure graft and patient outcomes. In addition, heavy administrative responsibilities (including paperwork and adherence to regulatory requirements) and high patient-to-provider ratios increase workload and reduce time for patient care.42 This creates a “pressure cooker” environment replete with a constant exposure to patient suffering. Moreover, providers and families often make decisions about a patient’s care without the patient’s involvement.43
Along with compromised work satisfaction, burnout also leads to depression, posttraumatic stress disorder, and substance use among health care professionals, which contributes to medical errors and provision of lower quality care.42 Burnout also leads to higher patient mortality rates and hospital-acquired infections,42 creating a vicious cycle. Discussing the existence and validity of burnout, as well as identifying sources of professional fulfillment and well-being, is crucial. A systems-based approach (including peer support and counseling) is needed to mitigate burnout44 for those experiencing moral distress and compassion fatigue. Education on coping mechanisms and resilience building should also be incorporated. Advocacy for changes in health care delivery, regulatory incentives, and reducing the burden of menial tasks should help to create a sustainable system that delivers quality care in a positive and supportive work environment.41
Are Clinicians Liable for Disregarding the Views of the Family or the Patient?
Clinicians have a professional responsibility to provide care that is in the best interest of their patients (based on medical evidence, ethical standards, and patient preferences whenever possible). However, on occasion, the views of the family or the patient conflict with what the clinician believes are medically appropriate and ethically sound.45,46 In such cases, the clinician’s primary obligation is to prioritize the well being and safety of the patient. This means that while the clinician should account for the wishes and preferences of the patient and their family, they may need to make decisions that go against these views if they believe it is necessary to protect the patient’s health.
Liability can arise if a clinician fails to adhere to accepted medical standards or acts negligently, thereby resulting in harm to the patient. However, if a clinician’s actions are based on sound medical judgment and ethical principles, even if those actions go against the wishes of the patient or family, they are generally protected from liability. This is important when addressing issues of medical futility. Overall, the principle of medical futility aims to ensure that health care resources are used effectively and that patients receive treatments that are likely to provide meaningful benefits in terms of health outcomes and quality of life.
A common mistake that physicians make when approaching the family members of a critically ill patient who lacks the capacity to make medical decisions is asking “What would you like me to do?” The implication of this question shifts the locus of control from the patient to the patient’s family members. If a critical care physician suggests discontinuing care (eg, artificial ventilation), the patient’s family may hear the question “Do you want me to stop the ventilator?” as “Do you want me to let your father die?”
To honor the principle of autonomy, a better question to ask would be “Given everything I shared with you, if your dad could speak, what do you think he would want me to do?” That returns the locus of control back to the patient. In the end, the goal is to understand what the patient would like to do under these circumstances, not what their family members would like the doctors to do. Under most circumstances where there are relatively healthy familial relationships, the patient’s family would mostly like the doctors to do anything within their power to save his life. Clinicians should document their decision making process thoroughly, especially when there is disagreement with the patient or family, to demonstrate that their actions were based on professional standards and the best interests of the patient.
What Happened to Ms A?
Ms A’s care, at the time of this writing, continues to be complicated. Her caregivers identified and voiced their strong feelings and opinions during multiple multidisciplinary and family meetings. Given that Ms A has been delirious and continues to lack capacity to make medical decisions, her family has been acting as her surrogate decision-maker. Multiple teams conferred and concluded that for now, although Ms A is indeed very ill, she is stable and has some, but minimal, hope for recovery. The family and teams decided to continue care until either a catastrophic event occurs, the teams decide that her care has become futile, she regains the ability to communicate effectively and indicates her desire to withdraw care, or her family (as surrogate decision makers) decides to change her course of care.
In addition to clinical meetings, multiple meetings were held, including some with the trainees who have been caring for this patient, to process the difficult feelings and thoughts evoked by caring for Ms A. Clinicians shared their feelings of helplessness, frustration, anger, compassion, and care, as well as their admiration for the family’s tenacity. They expressed their wishes for their own end-of-life care. These discussions facilitated personal growth for all involved; they continue to be fully engaged in the care of Ms A.
CONCLUSION
Our case illustrates the complexity, intensity, and critical decision-making faced by health care staff while caring for someone who is chronically and critically ill. Such complex cases can make staff feel like their efforts are futile, adding to the emotional and ethical burden that leads to burnout. By acknowledging the profound impact of these high-stress situations and the heavy burdens placed on health care workers, the root causes of burnout can be addressed (eg, implementing supportive systems, fostering professional fulfillment, and advocating for systemic changes). Prioritizing the well-being of health care providers will enhance their quality of life and improve patient care and outcomes, which ultimately benefits the entire health care system.
Taking care of critically ill patients with prolonged complicated courses and uncertain chances for meaningful recovery can be challenging and demoralizing for the medical teams. The situation can be especially difficult when the medical teams disagree on prognosis and plan of care or when families hold a different point of view from those of the medical teams and when the patient is unable to articulate their wishes. At times, clinicians might even wish for their patient to die, fueled by their own feelings of hopelessness and helplessness on behalf of the patient and feeling that they are delivering futile care and are contributing to the patient’s suffering. This can further add to their feelings of guilt and create moral distress and burnout. When this happens, it is important to acknowledge and name these difficult feelings and thoughts, withholding your judgement towards them. These feelings and thoughts can guide one’s understanding of the case and openly acknowledging them will help a clinician separate one’s critical assessment of the situation versus the projection of their own values and wishes towards end of life, realizing that the patient and family might indeed have different values.
It is then important to work with members of the multidisciplinary team and the family to understand and articulate the viewpoints of all the parties. If the patient is a transplant recipient, it is important to recognize that additional factors might contribute to the patient’s course. If there is a concern that program metrics are unduly influencing the team’s plan of care, it is important to address these in multidisciplinary meetings. Additional hospital teams and resources, such as ethics consultation services, can be particularly important in these complicated discussions.
At the end of the day, the clinician’s responsibility is to the patient, to benefit the patient and to do no harm, as guided by the patient’s values and wishes. Existing advance directives can be very helpful if a patient is unable to communicate. If the patient lacks capacity, surrogate decision-makers can help medical teams decide on behalf of the patient, again guided by the patient’s values and wishes. There are also legal and ethical safeguards against providing futile medical care, although in some situations it can be challenging to determine what futile medical care involves. Finally, acknowledging the most challenging and distressing thoughts that a clinician might have regarding a patient’s care and approaching them in a systematic nonjudgmental way can be liberating and help guide the patient’s care, bring the medical team together, and facilitate professional and personal growth.
Article Information
Published Online: February 25, 2025. https://doi.org/10.4088/PCC.24f03823
© 2025 Physicians Postgraduate Press, Inc.
Submitted: June 30, 2024; accepted December 5, 2024.
To Cite: Sher Y, Hussain F, Hoover BJ, et al. Wishing that your patient would die: reasons and reactions. Prim Care Companion CNS Disord 2025;27(1):24f03823.
Author Affiliations: Psychiatry and Behavioral Sciences, Stanford University School of Medicine, Stanford, California (Sher, Hussain, Hoover, Gunther, Fishman, Zein, Maldonado); Department of Psychiatry, Massachusetts General Hospital and Harvard Medical School, Boston, Massachusetts (Stern).
Corresponding Author: Yelizaveta Sher, MD, Psychiatry and Behavioral Sciences, Stanford University School of Medicine, 401 Quarry Rd, MC 5718, Stanford, CA 94305 ([email protected]).
Drs Sher, Hussain, Hoover, Gunther, Fishman, and Zein are co-first authors. Drs Maldonado and Stern are co-senior authors.
Relevant Financial Support: None.
Funding/Support: None.
Clinical Points
- Medical futility occurs when the desired outcome, although possible, is overwhelmingly improbable.
- When patients or their family members dispute the determination of medical futility and are opposed to withdrawal of care, patient advocates or an ethics committee should become involved.
- Assessment of capacity requires a multifaceted approach that balances clinical assessment, communication strategies, ethical considerations, and legal frameworks.
- Tension between clinical complexities and the quality metrics of transplant programs can create significant ethical dilemmas.
- Acknowledgment of feelings evoked while caring for those with critical illness can help to guide actions instead of blindly reacting to them.
References (46)

- Bernat JL. Medical futility: definition, determination, and disputes in critical care. Neurocrit Care. 2005;2(2):198–205. PubMed CrossRef
- Schneiderman LJ. Defining medical futility and improving medical care. J Bioeth Inq. 2011;8(2):123–131.
- Cross SH, Kaufman BG, Quest TE, et al. National trends in hospice facility deaths in the United States, 2003–2017. J Pain Symptom Manage. 2021;61(2):350–357.
- Schneiderman LJ, Jecker NS, Jonsen AR. Medical futility: its meaning and ethical implications. Ann Intern Med. 1990;112(12):949–954. PubMed CrossRef
- Beecher HK. Report of the ad hoc committee of the Harvard Medical School to examine the definition of brain death: the definition of irreversible coma. Transplantation. 1968;7(3):204.
- Fischer D, Edlow BL, Giacino JT, et al. Neuroprognostication: a conceptual framework. Nat Rev Neurol. 2022;18(7):419–427.
- Luaute J, Maucort-Boulch D, Tell L, et al. Long-term outcomes of chronic minimally conscious and vegetative states. Neurology. 2010;75(3):246–252. PubMed CrossRef
- Sokol DK. The slipperiness of futility. BMJ. 2009;338:b222. PubMed
- Olmstead JA, Dahnke MD. The need for an effective process to resolve conflicts over medical futility: a case study and analysis. Crit Care Nurse. 2016;36(6):13–23. PubMed CrossRef
- Curtis JR. Communicating about end-of-life care with patients and families in the intensive care unit. Crit Care Clin. 2004;20(3):363–380. PubMed CrossRef
- Akkermans A, Lamerichs JMWJ, Schultz MJ, et al. How doctors actually (do not) involve families in decisions to continue or discontinue life-sustaining treatment in neonatal, pediatric, and adult intensive care: a qualitative study. Palliat Med. 2021;35(10):1865–1877.
- Kon AA, Davidson JE, Morrison W, et al. Shared decision making in ICUs: an American college of Critical Care Medicine and American Thoracic Society policy statement. Crit Care Med. 2016;44(1):188–201.
- Gan JM, Riley J, Basting R, et al. Decision-making capacity in older medical in patients: frequency of assessment and rates of incapacity by decision-type and underlying brain/mind impairment. Age Ageing. 2023;52(9):afad171.
- Moore RF. A guide to the assessment and care of the patient whose medical decision-making capacity is in question. Med Gen Med. 1999:E7.
- Porrino P, Falcone Y, Agosta L, et al. Informed consent in older medical inpatients: assessment of decision-making capacity. J Am Geriatr Soc. 2015;63(11):2423–2424. PubMed CrossRef
- OPTN Enhanced Transplant Program Performance Metrics. 2022. Accessed July 16, 2024. https://optn.transplant.hrsa.gov/media/r5lmmgcl/mpsc_performancemetrics_3242022b.pdf
- Saramoriarty. Two new transplant performance metrics to implement July 14, 2022, UNOS. 2022. Accessed July 16, 2024. https://unos.org/news/two-newtransplant-performance-metrics-to-implement-july-14-2022/
- Courtwright AM, Rubin E, Robinson EM, et al. An ethical framework for the care of patients with prolonged hospitalization following lung transplantation. HEC Forum. 2019;31(1):49–62.
- 2020 U.S. organ and tissue transplants: cost estimates, discussion, and emerging issues. Milliman. 2020. Accessed July 16, 2024. https://www.milliman.com/en/insight/2020-us-organ-and-tissue-transplants
- Nelson JE, Cox CE, Hope AA, et al. Chronic critical illness. Am J Respir Crit Care Med. 2010;182(4):446–454. PubMed
- Goold SD, Williams B, Arnold RM. Conflicts regarding decisions to limit treatment: a differential diagnosis. JAMA. 2000;283(7):909–914. PubMed CrossRef
- Baldwin DC Jr, Daugherty S. Interprofessional conflict and medical errors: results of a national multi-specialty survey of hospital residents in the US. J Interprof Care. 2008;22(6):573–586. PubMed CrossRef
- Fassier T, Azoulay E. Conflicts and communication gaps in the intensive care unit. Curr Opin Crit Care. 2010;16(6):654–665. PubMed CrossRef
- Savel RH, Munro CL. Conflict management in the intensive care unit. Am J Crit Care. 2013;22(4):277–280. PubMed CrossRef
- Honiden S, Possick J. Should physicians new to a case, counsel patients and their families to change course at the end of life? AMA J Ethics. 2018;20(8):E699–E707. PubMed CrossRef
- Aulisio MP, Chaitin E, Arnold RM. Ethics and palliative care consultation in the intensive care unit. Crit Care Clin. 2004;20(3):505–523. PubMed CrossRef
- Curtis JR, Vincent JL. Ethics and end-of-life care for adults in the intensive care unit. The Lancet. 2010;376(9749):1347–1353. PubMed CrossRef
- Mercadante S, Gregoretti C, Cortegiani A. Palliative care in intensive care units: why, where, what, who, when, how. BMC Anesthesiol. 2018;18(1):106. PubMed CrossRef
- AMA-Code. Medically ineffective interventions. Accessed October 2, 2025. https://code-medical-ethics.ama-assn.org/ethics-opinions/medically-ineffectiveinterventions
- Bosslet GT, Pope TM, Rubenfeld GD, et al. An Official ATS/AACN/ACCP/ESICM/ SCCM Policy Statement: responding to requests for potentially inappropriate treatments in intensive care units. Am J Respir Crit Care Med. 2015;191(11):1318–1330. PubMed
- McCabe MS, Storm C. When doctors and patients disagree about medical futility. JOP. 2008;4(4):207–209. PubMed CrossRef
- Teno JM, Gozalo P, Trivedi AN, et al. Site of death, place of care, and health care transitions among US Medicare beneficiaries, 2000-2015. JAMA. 2018;320(3):264–271. PubMed
- Furuno JP, Noble BN, McPherson ML, et al. Variation in hospice patient and admission characteristics by referral location. Med Care. 2020;58(12):1069–1074. PubMed CrossRef
- Mack JW, Cronin A, Taback N, et al. End-of-life care discussions among patients with advanced cancer: a cohort study. Ann Intern Med. 2012;156(3):204–210. PubMed CrossRef
- House SA, Schoo C, Ogilvie WA. Advance directives. StatPearls Publishing Copyright © 2024. StatPearls Publishing LLC; 2024.
- Rietjens JAC, Sudore RL, Connolly M, et al. Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care. Lancet Oncol. 2017;18(9):e543–e551. PubMed
- McMahan RD, Tellez I, Sudore RL. Deconstructing the complexities of advance care planning outcomes: what do we know and where do we go? A scoping review. J Am Geriatr Soc. 2021;69(1):234–244.
- Morrison RS, Meier DE, Arnold RM. What’s wrong with advance care planning? JAMA. 2021;326(16):1575–1576. PubMed
- Malhotra C, Ramakrishnan C, Yue SMG. Challenges in providing end-of-life care consistent with documented patient preferences. Ann Palliat Med. 2022;11(12):3610–3619.
- Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. PubMed CrossRef
- Niven AS, Sessler CN. Supporting professionals in critical care medicine: burnout, resiliency, and system-level change. Clin Chest Med. 2022;43(3):563–577.
- Moss M, Good VS, Gozal D, et al. A Critical Care Societies Collaborative Statement: burnout syndrome in critical care healthcare professionals. A call for action. Am J Respir Crit Care Med. 2016;194(1):106–113. PubMed
- Flannery L, Ramjan LM, Peters K. End-of-life decisions in the intensive care unit (ICU) - exploring the experiences of ICU nurses and doctors - a critical literature review. Aust Crit Care. 2016;29(2):97–103. PubMed CrossRef
- Bateman ME, Hammer R, Byrne A, et al. Death Cafés for prevention of burnout in intensive care unit employees: study protocol for a randomized controlled trial (STOPTHEBURN). Trials. 2020;21(1):1019.
- Beauchamp TL, Childress JF. Principles of Biomedical Ethics. Oxford University Press; 2019.
- Davies B. Responsibility and the limits of patient choice. Bioethics. 2020;34(5):459–466. PubMed CrossRef
Enjoy this premium PDF as part of your membership benefits!